Crowns provide a viable solution for patients who require significant restorative work due to extensive decay. When nearly an entire arch of teeth requires crowns, collaboration between the dentist and dental lab is crucial for optimal patient results. As the industry barrels towards digital workflows and processes, dentists still want the same thing – predictable outcomes for their patients.
In the case that follows, I will outline the process by which I delivered 10 maxillary crowns for a patient with subgingival margins and generalized gingivitis.
Patient presentation
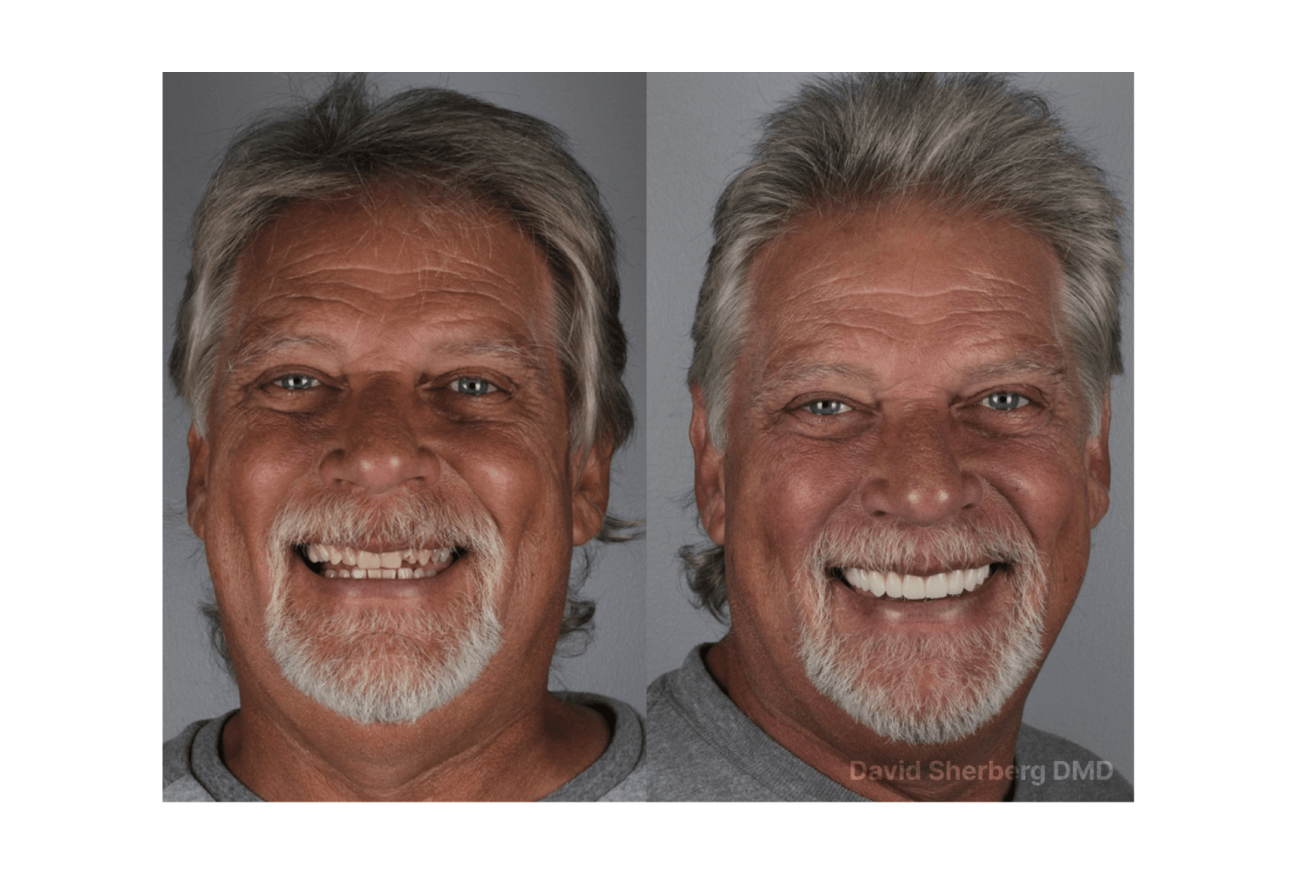
Figures 1a, 1b, 1c:
Figures 1a, 1b, 1c: The patient’s dentition upon visual inspection reveals extensive decay and inflamed gingiva.
In the case discussed here, a 58-year-old male-identifying patient presented to the practice complaining that he hated the look of his smile and his “bleeding, boggy gums,” and that this has been something he has been aware of for about 20 years. Upon examination, the patient presented with generalized gingivitis as well as several instances of subgingival decay.
With consideration for both the patient’s gingivitis and subgingival decay, we opted to restore with 10 zirconia translucent aesthetic crowns on teeth #4-13.
Case description
Appointment #1:
The patient first received a cleaning in which Strupp’s chlorhexidine irrigation protocol was followed to clean the gingiva as much as possible. Following the cleaning, the gums still appeared edematous and erythematous, but were manageable enough to move forward with the next step. Intraoral scans of the patient’s upper and lower arches and bite were then captured. These scans were sent to Dandy with a request to have a Digital Design Preview created for review.
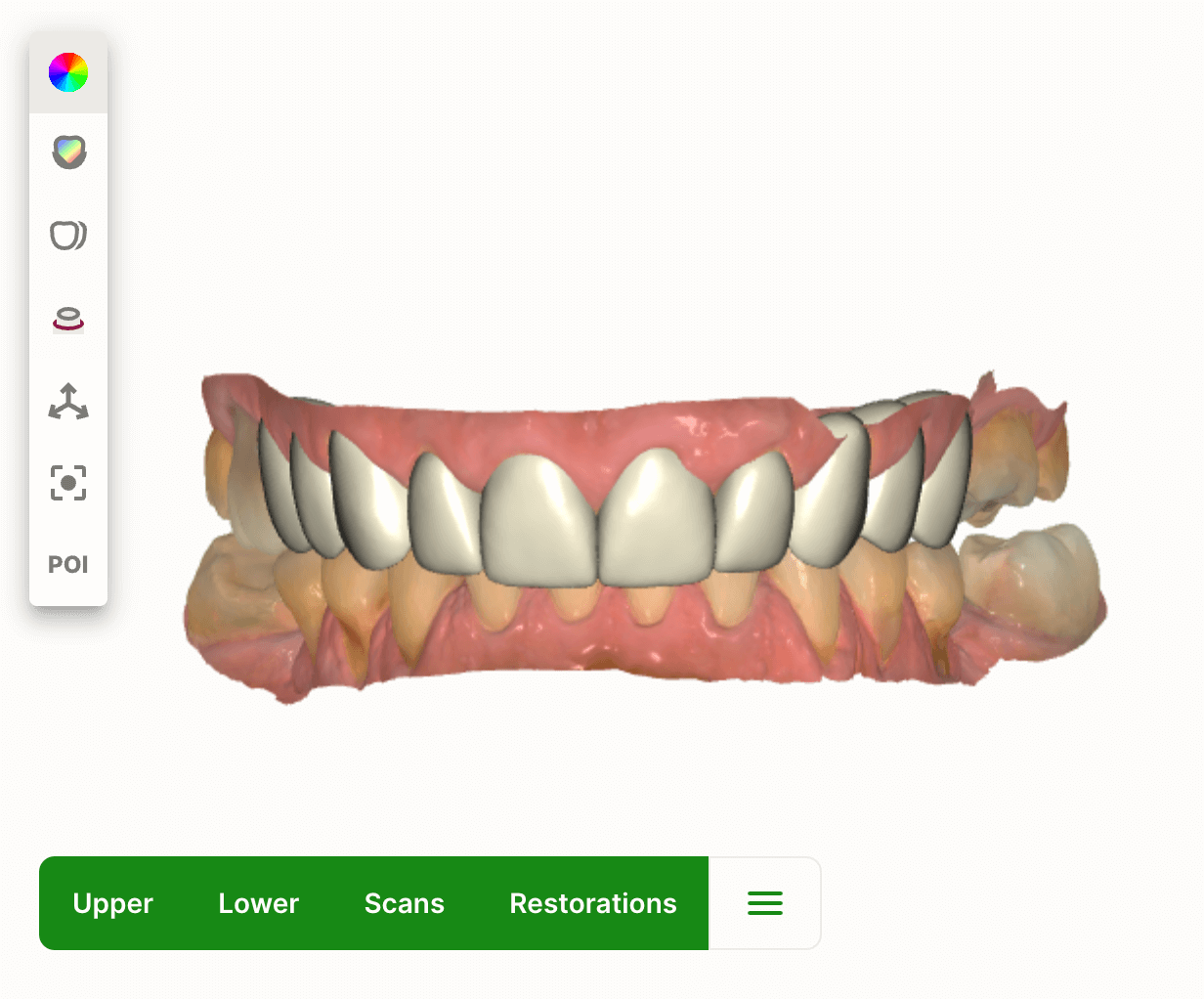
In between the first and second appointments, the Digital Design Preview was created (Fig. 2). Upon review and approval of the digital preview, a model was ordered. The model was used to make PVS stents for future reduction guides and eventual temporary crowns.
Figure 2: The Digital Design Preview was used to preview the proposed anatomy of the model. Once moving forward with an approved design, this model would be used for in-office creation of reduction guides and the first set of temporaries.
Appointment #2:
With the patient under oral conscious sedation (OCS), teeth #4-13 were prepped and notable caries control was required. Buildups were required and performed on certain teeth as needed. Due to expected carious exposure during treatment, teeth #10 and #12 would also require endodontic treatment in a subsequent appointment. New intraoral scans were captured for imaging of the prepped teeth. Gingival retraction was performed for margin visibility for the scanner with the understanding that the gingivitis and subgingival decay would prevent perfect visibility. Instead, having closed margins was deemed more important than visible margins at this stage of treatment. Teeth #4-13 were temporized.
Appointment #3:
The focus of treatment was shifted to the endodontic needs of teeth #10 and #12 in addition to the patient’s gingival health. Endodontic treatment was performed successfully on teeth #10 and #12. The existing temporary crowns then were removed from teeth #4-13. New temporary crowns were 3D-printed in-office on a Phrozen Sonic Mini 4K using Rodin Sculpture resin and delivered (Fig. 3). The fit of these new temporary crowns was quite accurate, requiring only minor interproximal adjustments and minor occlusal equilibration. The patient requested that the shade of the final crowns be whiter. With these temporary crowns seated, attention could be given to managing the patient’s gingival health.
After this third appointment, the patient returned for two additional irrigation sessions, following the Strupp protocol. The patient was also instructed on at-home oral hygiene best practices with an emphasis on brushing and flossing well. The patient’s gingival health appeared significantly healthier after the second irrigation session.
Figure 3: The patient’s second set of temporaries that were 3D-printed in-office. The anatomy of these temporaries was ideal, and ultimately replicated by Dandy when designing and fabricating the final crowns.

Appointment #4:
Intraoral scans of the temporary crowns were captured in order to have their anatomy copied exactly for the final crowns. The temporary crowns on teeth #4-13 were removed, and the underlying crown preps were finalized. Because each tooth’s margin was subgingival, meticulous retraction was performed with a double-cord technique using the following cord sizes:
- Posterior teeth: #00 followed by #1 cord
- Anterior teeth: #000 followed by #00 cord
To capture these scans accurately, the top cords of 2-3 teeth were pulled at a time, and then these teeth immediately were scanned. These scans were then locked using the Lock Tool on Dandy’s Chairside software. From there, the top cords of the next few teeth were removed, scans of these teeth were captured, and the scans were locked. This cord-pull, scan, and lock technique was repeated until all treated teeth were captured.
Both the scans of the temporary crowns and the crown preps were sent to Dandy. A Digital Design Preview and zirconia translucent aesthetic crowns were ordered. A note was included that the anatomy of the temporary crowns should be copied and no changes should be made without my approval. In terms of shade, a darker gingival third was requested as well. The temporary crowns were cemented back onto teeth #4-13.
After this fourth appointment, the Digital Design Preview was received and the proposed design was approved (Fig 4a, 4b). The subgingival nature of this case impacted margin visibility, so I connected with Dandy’s Clinical Support Team to identify and confirm the location of each margin of each crown.
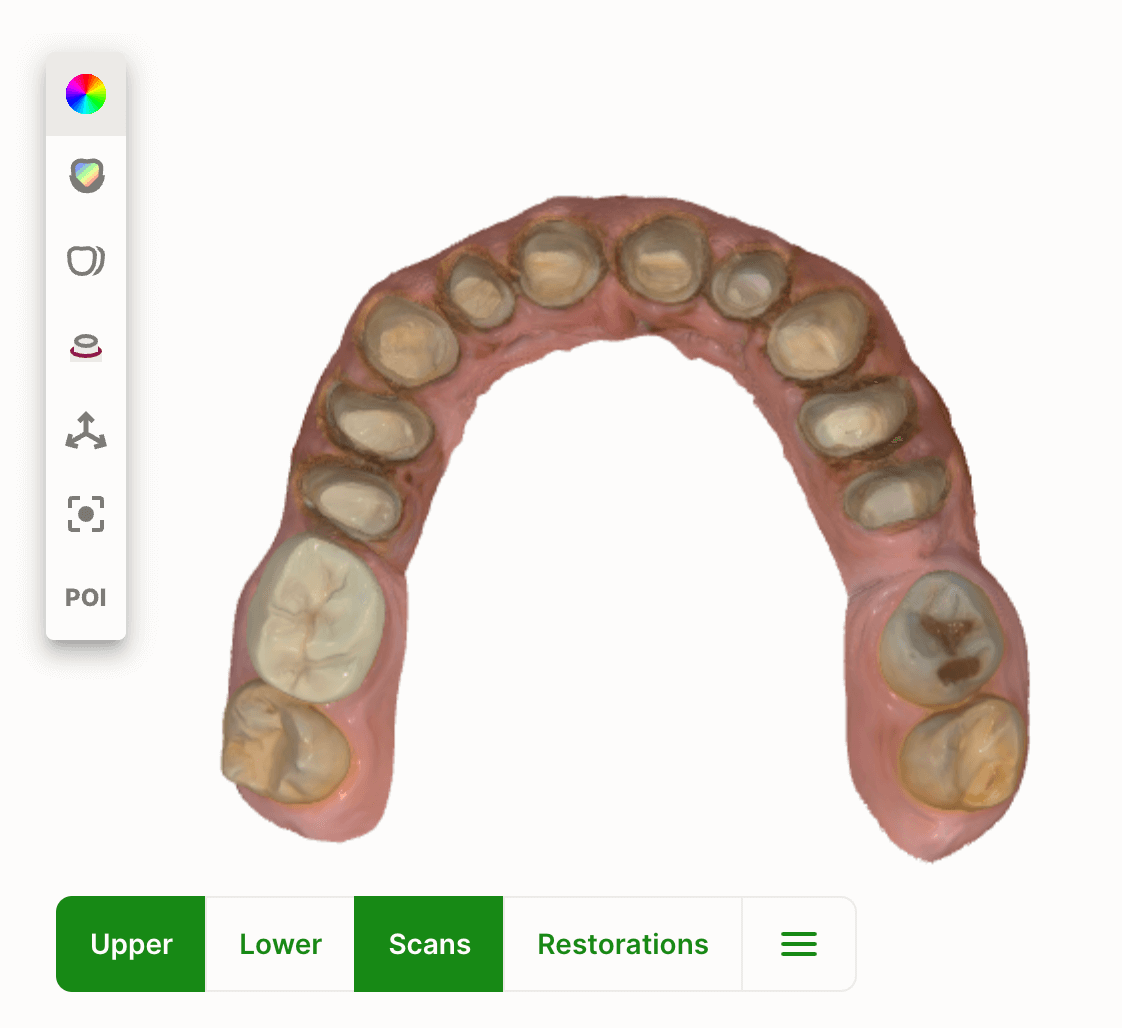
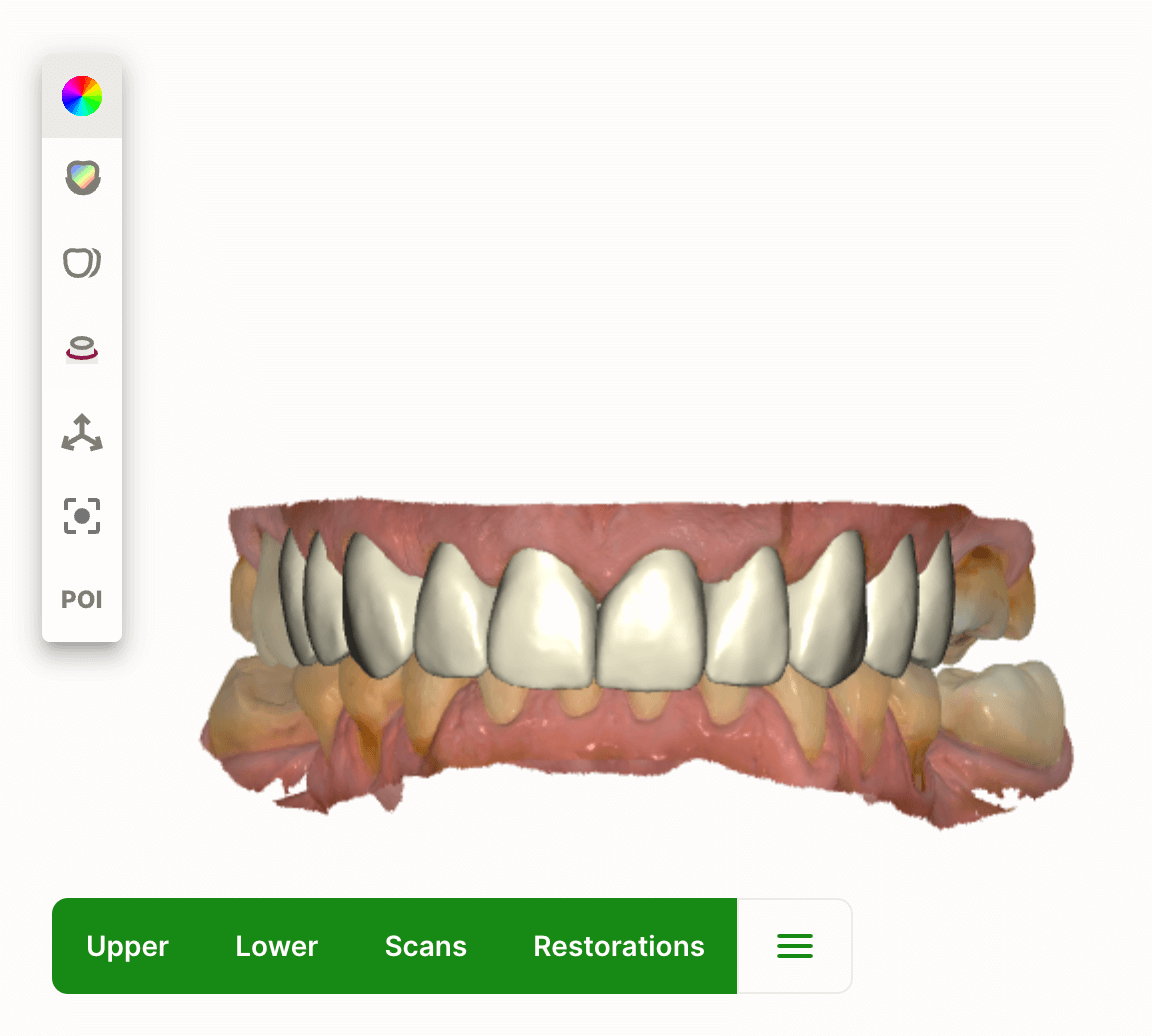
Figure 4a, 4b: The next set of Digital Design Previews displays the scans of the crowns and the proposed final crown design. This Digital Design Preview allowed for alignment between dentist and lab on final restoration design.
Appointment #5:
Zirconia translucent aesthetic crowns were delivered on teeth #4-13 using Fuji-Cem (Fig. 5). Very minor interproximal and occlusal adjustments were required.
Figure 5: The delivered final crowns. Note the aesthetic quality. It is helpful to provide Dandy with cosmetic instructions such as varying shades (i.e. gingival, middle, and incisal thirds), leaving texturing instead of high polishing, etc.

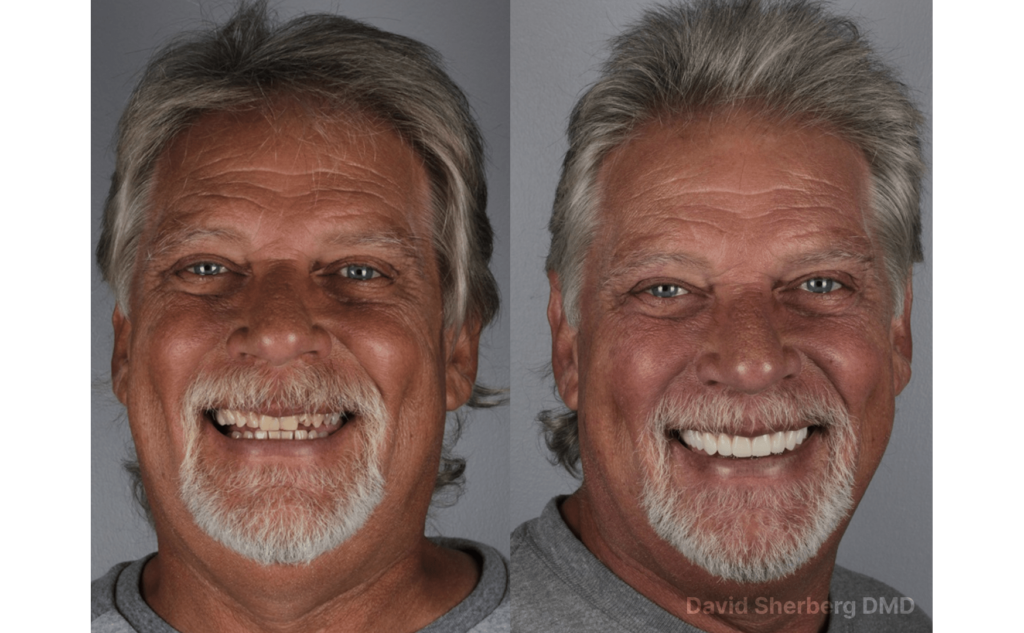
Patient before and after
Dandy’s technology
Dandy’s Digital Design Preview allowed for specific and clear communication with Dandy throughout the various stages of treatment. This communication and visualization tool allowed each step of the diagnostic, design, and treatment process to be definitively analyzed and accounted for—ultimately leading to a smooth delivery appointment for such an aesthetic and involved case. Thanks to the Digital Design Preview the patient outcome and experience were ideal.
In addition to the Digital Design Preview, collaborating directly with the Clinical Support Team personalized my communication with Dandy. This team provided one-on-one support so that the nuanced but critical details of this case could be incorporated into the final restorations.
Conclusion & best practices
With digital dentistry, subgingival margins can be especially challenging, especially when managing gingival health. On top of that, factoring in aesthetics and a near-entire arch of crowns, and you’re looking at a massive challenge. Using Dandy’s technology to coordinate and collaborate among patient needs, treatment recommendations, and final design brings a case like this to life. In the end, subgingival crown cases require their own level of meticulousness, but even in a digital workflow, returning to the fundamental principles of proper gingival retraction, hemostasis, and direct communication with your lab leads to excellent results.
About the author
Dr. David Sherberg is a resident of St. Petersburg, FL. He founded Bayway Dental with the goal of providing most, if not all, dental services for his patients right at his office. After graduating from the University of Connecticut School of Dental Medicine, Dr. Sherberg opted to continue his education with an Advanced Education in General Dentistry Residency at Virginia Commonwealth University. He has received extensive dental implant continuing education, including the Comprehensive Interdisciplinary Dental Implant Certification at the University of Florida, Full Arch Guided Surgery, and Immediate Teeth (Same Day Teeth®) training from The Pikos Institute, and membership in the International Congress of Oral Implantologists. As a testament to his commitment to excellence in IV sedation dentistry, he is a certified DOCS Education member.




