According to a study by the American Academy of Sleep Medicine (AASM), 29.4 million Americans are affected by obstructive sleep apnea–approximately 12 percent of the US adult population. For a good number of these people, an oral sleep apnea appliance is a great treatment—and one they will stick with. As a dentist, you can now play a part in the sleep apnea battle by fitting an oral appliance to your patient.
People with untreated sleep apnea have an increased risk of health complications including hypertension, diabetes, heart disease, and depression. Obstructive sleep apnea (OSA) is a sleep-related breathing disorder in which a person experiences an obstruction to the upper airway during sleep.
Common signs of sleep apnea include:
- Gasping or choking during sleep
- Snoring
- Fatigue or sleepiness while awake
- Impaired cognitive function
Dentists can check patients for signs of sleep apnea when performing an oral exam. Anatomical features such as a high-arched palate, large neck circumference, large tongue, large tonsils, or craniofacial structure can contribute to sleep apnea. If a patient’s partner or family member mentions that the patient chokes, gasps, snores loudly, or stops breathing during sleep, these may be signs of sleep apnea.
Patients with these symptoms should be referred to a primary care physician or a sleep medicine specialist for further examination.
If a doctor or specialist determines that a dental device is required, a qualified dentist will take a scan or impression of the patient’s mouth to make a sleep apnea oral appliance. That is then sent to a dental lab for custom device fabrication. When the appliance is completed, the patient returns to the dentist’s office for further adjustments.
Dentists who work collaboratively with a patient’s primary care physician and sleep physician provide the best care for their OSA patients.
Sleep apnea with Dandy
Dentists can offer both the Herbst and the Dorsal intraoral device for sleep apnea with Dandy. Both products are 3D printed to ensure a high level of accuracy and comfort. This ensures a high degree of efficacy when treating sleep apnea.
Traditional treatment for sleep apnea
OSA is a result of anatomical structures constricting airways (i.e. large neck circumference, large tonsils, obesity, etc.). Breathing’s partial blockage (hypopnea) and complete stoppage (apnea) may last from several seconds to more than a minute.
Diagnosis of OSA and its degree of severity are determined by a sleep study measuring patients’ apnea-hypopnea index (AHI), that is, the combined average number of apneas and hypopnea events that occur per hour of sleep. OSA severity is categorized into three tiers:
- Mild (5-15 events/hour)
- Moderate (15-30 events/hr)
- Severe (> 30 events/hr)
It is important to note that even mild cases of OSA can impact the sufferer’s health and quality of life. Symptoms of mild sleep apnea can include:
- Daytime exhaustion
- Difficulty concentrating
- Memory issues
- Reduced libido
- Mood disorders
- Complications with anesthesia during medical procedures
- Reduced reaction-time when driving or operating machinery
- Nocturnal bruxism
- Insomnia
- Increased strain on relationships.
It is not an understatement to say that treating OSA can change patients’ lives significantly, leading to improved overall health, relationships, and work productivity.
Traditionally, some of OSA’s treatments have included patient-motivated lifestyle changes such as:
- Weight loss
- Diet changes
- Smoking and alcohol cessation
Such lifestyle changes may only prove out over time, may have limited effectiveness, and can carry high risk of abandonment.
Craniofacial/maxillofacial surgery has been used to effectively treat OSA, but these surgeries are often onerous to patients considering their cost, painful and uncomfortable recovery periods, and potential changes to the patient’s physical appearance.
The most common and reliably prescribed traditional OSA treatment is nightly use of a continuous positive airway pressure (CPAP) machine–a motorized device that keeps airways open by supplying a constant flow of air through the nose, mouth, or both via a mask worn over the face during sleep.
The rise of the sleep apnea oral appliance
The practice of manipulating anatomy to unblock an otherwise constricted airway has been common practice in anesthesiology for decades; sleep apnea dental appliances work according to the same proven principles. Studies have shown that sleep apnea oral appliances can be an effective alternative for those who cannot tolerate a CPAP.
While pre-made dental devices for sleep apnea can be found in online marketplaces, these are, more often than not, imprecise, cheaply made, and uncomfortable with limited-to-no ability for adjustment. Studies show higher rates of device failure and user abandonment with these thermoplastic appliances compared to custom-made ones. Furthermore, these so-called “boil and bite” appliances are available without a dentist consultation; treatment predicated on self-diagnosis may fail to remediate the condition and/or cause entirely new jaw and bite issues.
By contrast, today’s digital dental labs and scanning technology have profoundly refined the fit and fabrication process for sleep apnea dental appliances. Most patients do not know that obtaining a superior product that is lighter, sturdier, more durable, more comfortable, and tailored to their specific needs is easier than ever. Furthermore, it bears stating that, as a dentist, you can check-in on patients’ progress with their oral appliance, making you an instrumental part of this life-changing treatment.
Oral appliance for sleep apnea vs. CPAP therapy
The goal of both CPAP and dental devices for sleep apnea are the same: Keep airways clear during sleep. However, the choice of which route to take depends on the individual–their needs and tolerances and anatomy.
Every CPAP machine consists of three components: mask, hose, and the machine itself. The machine pumps air through the hose to the mask worn around the sleeper’s face. Each machine has its own options, interface, and controls that must be mastered for proper use.
There are three primary types of CPAP:
- Traditional CPAPs supply constant air pressure.
- Auto-adjusting machines raise or lower pressure according to the user’s breathing patterns.
- Bilevel machines toggle between high and low pressure during inhale and exhale, respectively.
There are also many different styles of mask, but three primary types:
- Full-face masks cover both the nose and mouth
- Nasal masks fit over the nose
- Nasal pillows fit directly into the nostrils
By contrast, oral devices consist of very few parts: either a single piece worn in the mouth or two connected pieces worn on the top and bottom jaw. There are different types of oral devices, but all work by adjusting and/or immobilizing anatomical structure.
Comfort
CPAP: Regardless of the type of CPAP mask used, the business end will still need to be secured to the head via a strap or headgear. In addition, the mask must always have uninterrupted connection to the hose, and the hose to the machine, effectively tethering the user’s head. This may feel uncomfortable for users. All CPAPs are effective, but none run silently–if a patient or a partner are sensitive to noise during the night, they (along with 30% to 50% of patients) may find a PAP machine difficult to tolerate. Finally, while advancing technology has shrunk their size to about that of a tissue box, CPAP machines still require users to find space to fit the machine for optimal airflow and user comfort, which may present a challenge for those with limited bedroom space.
Oral appliance: There are several different varieties of custom dental device for sleep apnea, but all fit into a user’s mouth much like a retainer or mouth guard, or in the case of tongue retaining devices, pacifier. There are no moving parts, harnesses, or additional pieces of equipment. The user is free to move during sleep and all the devices are silent.
Maintenance
CPAP: As they constantly blow air, most CPAP machines have a built-in humidifier to prevent users from dehydrating during sleep. However, these CPAPs must be supplied with fresh distilled water; tap or conventionally filtered water are not recommended as they may contain minerals or bacteria that can not only damage or contaminate the machine, but the user as well. CPAPs (including hoses and masks) must also be cleaned weekly (at a minimum) in order to keep the machine in working order and prevent buildup of dangerous allergens, mold, and bacteria. Finally, as a CPAP has electronic, software, and motorized components all working together, like any machine from car to PC, error or failure in one or all of these systems requires troubleshooting, maintenance, or even replacement.
Oral appliance: Keeping a dental device for sleep apnea clean and bacteria-free is easy. On a daily basis, the patient is simply required to brush and floss before use. In the morning, give the device a once-over with a soft-bristled brush before storing it a clean, dry box. Both the box and the device require a weekly deep cleaning, but, depending on the device’s material components, that usually just consists of a soak with denture tablets or in white vinegar solution.
Convenience
CPAP: Like a desktop computer, home CPAPs can be transported, but doing so is cumbersome and inconvenient. If a patient is sleeping away from home, there are indeed excellent smaller, travel-sized CPAP devices, but these still require the user to wear a mask connected to a hose. Note that these miniaturized devices often lack important quality-of-life features (e.g. limited air pressure, no humidifier) and can be costly as they are not typically covered by insurance. Finally, CPAPs of any kind are difficult to use in transit (e.g. overnight flights, buses, or trains) or communal sleep settings (e.g. dorms, road trips, hostels) where space is limited and their operation can disturb others.
Oral appliance: Dental devices for sleep apnea fit in the palm of your hand and can slip right into a purse, backpack, or even pocket. Since patients are transporting one single device with no accouterments (besides a small clamshell carrying case), there is no interruption in the quality of treatment at home versus on the go. Finally, since there are no moving parts and they take up no extra space, they are convenient to pop in in any setting from camping tent to trans-continental flight.
The benefits of an oral appliance for sleep apnea
The best oral appliance for sleep apnea is one that patients will use consistently, and studies have shown that, in general, patients tend to stick with custom made oral appliances over both off-the-shelf alternatives and CPAPs.
The benefits of custom made oral appliances include:
- Increased sleep quality – Eliminating snoring and obstructed breathing leads to more restful nights and improved daytime functioning.
- Easy and straightforward use – With no extra equipment or parts, a user simply has to insert the device into their mouth.
- Higher comfort – Users who find the over-the-head harness, equipment over their face and/or tether to the machine uncomfortable often find an oral appliance much easier to tolerate. Oral devices are also silent, so no worrying about disturbing a partner.
- Individualized treatment – Since they are fabricated according to the user’s own anatomy in consultation with a dental professional, those who opt for a custom appliance can be assured that their specific needs and preferences are baked into the device, so to speak.
- Convenience – Oral devices can fit virtually anywhere and only require daily brushing and weekly soaking for maintenance.
The disadvantages of oral appliances for sleep apnea
No treatment of any medical condition is free from drawbacks, and sleep apnea dental appliances are no different. Simply put, there are those for whom an oral device is not an option and for those who do opt for the treatment, there may be side effects.
Patients who have loose teeth or advanced periodontal disease should not use an oral appliance as it could exacerbate or complicate the condition. The anatomy of those who are under 18 years of age may still change, so it’s not advisable for them to use an oral device. It is possible that use of an oral appliance for sleep apnea can change the position of users’ teeth or bite, sometimes permanently. It is also possible that sleeping with a device held in the mouth can lead to excess salivation, obstruction of oral breathing; gingival, dental, and/or temporomandibular joint pain/soreness.
It is of paramount importance that the root-cause and severity of a patient’s sleep apnea is determined before prescription of an oral appliance as there are serious contraindications:
- Severe sleep apnea (AHI > 30)
- Central sleep apnea (i.e. neurophysiological)
- Complex sleep apnea (i.e. central comorbid with obstructive)
- Sleep apnea resulting from morbid obesity
To reduce the risks of complications, dentists should take a patient’s full medical history including any history of asthma, breathing, respiratory disorders, or other relevant health problems.
Finally, it should be noted that, while oral devices for sleep apnea are shown to be as efficacious in reducing the severity of OSA as CPAP on average, this may be attributable to the inferior compliance of CPAP compared to oral devices. One out of three users of a dental device for sleep apnea experience negligible improvement of their symptoms which, compared to CPAP, makes them a less reliable treatment.
Oral appliances for sleep apnea therapy: How do they work and what role does a dentist play?
OSA most commonly occurs because soft tissue naturally relaxes during sleep, collapsing into airways, making normal respiration difficult if not impossible. The tongue may fall back occluding the airway, the mandible may be underdeveloped or positioned too far back, smoking might cause inflammation, alcohol consumption may lead to excessive relaxation of throat muscles, a patient’s congenital craniofacial structure may narrow airways–as there is no single cause of the condition, there is no one-size-fits-all solution.
Oral appliances are devices that help to reduce physical blockages of the airway. They are placed in the mouth to help keep the airway open while the patient sleeps. The appropriate device is predicated on the root-cause of a patient’s sleep apnea. As a dentist, you can play a crucial role in diagnosing a patient’s sleep apnea by:
- Evaluating patients for OSA
- Evaluating patients for the suitability of an OSA appliance
- Choosing the most appropriate oral appliance for the patient
- Facilitating device fabrication
- Follow up: Adjusting thr appliance or assessing patients for possible adverse effects.
There is no objectively ‘best’ oral appliance for sleep apnea, only the one that’s best suited to the individual.
Types of oral appliances for sleep apnea
There are different categories of oral devices for adults with sleep apnea, each with its own mode of action: Soft palate lifters, Tongue retaining devices (TRDs), and mandibular advancement devices (MADs) also known as mandibular advancement appliances (MAAs) mandibular repositioning appliances (MRAs) or mandibular advancement splints (MASs).
Soft palate lifters elevate the soft palate and uvula, but are least effective of the three. TRDs are worn at the front of the mouth between the lips and use suction to hold the tongue forward, preventing it from falling back into the airway. These devices are shown to be effective, but less than others. MADs are the most effective and therefore most commonly prescribed of the three and as such, MADs are considered by some to be best oral appliance for sleep apnea. However, again, ‘best’ is subjective and effectiveness depends on the patient and their individual needs.
Mandibular advancement devices
MAD is an oral appliance that keeps the mandible and the tongue in a protruded position, widening the upper respiratory tract. This prevents the patient’s airway from collapsing during sleep. A MAD is placed in the mouth before sleep. The appliance is removed when the patient wakes.
Tongue-Stabilizing Device (TSD)
A tongue-stabilizing device, often called a tongue-retaining device, uses suction to move the tongue forward during sleep to keep the tongue from blocking the airway. During use, the tip of the patient’s tongue protrudes through the lips. Research suggests that TSDs may reduce breathing lapses.
Mouth guards
Over-the-counter sleep guards are similar to mandibular advancement devices, they attempt to work by repositioning the lower jaw forward to keep the airway clear while the patient sleeps. Mouth guards are available without a prescription and sold in pharmacies or online. The patient immerses the mouth guard in a cup of boiling water for 60 seconds and firmly bites down on the softened plastic to create a custom-made impression. While these devices are the lowest barrier to entry, they run the inherent risk of the patient not creating a good bite in the mold they make at home.
Rapid Maxillary Expansion (RME)
For children with OSA, rapid maxillary expansion (RME) is an orthodontic device that opens the airway by expanding the roof of the mouth. The child wears a custom-fitted expander, which is placed over the upper molars. The child wears the RME continuously. RMEs are designed to adjust the airway of children who have highly arched or narrow hard palates. Studies suggest that RME combined with surgery for tonsil removal or adenoid removal is more effective than RME treatment alone.
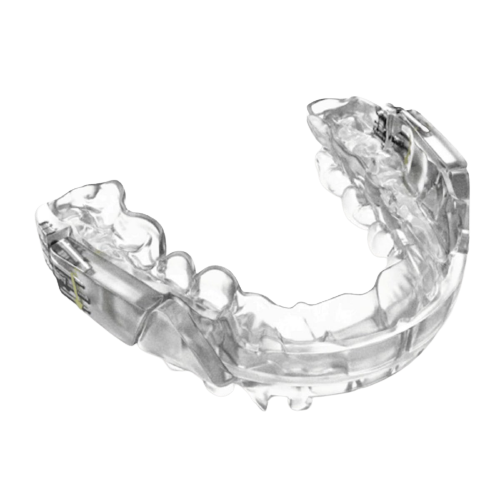
Popular oral appliances for sleep apnea from Dandy
Dandy’s digital labs create custom 3D printing MADs sleep apnea devices that may best treat your patient.
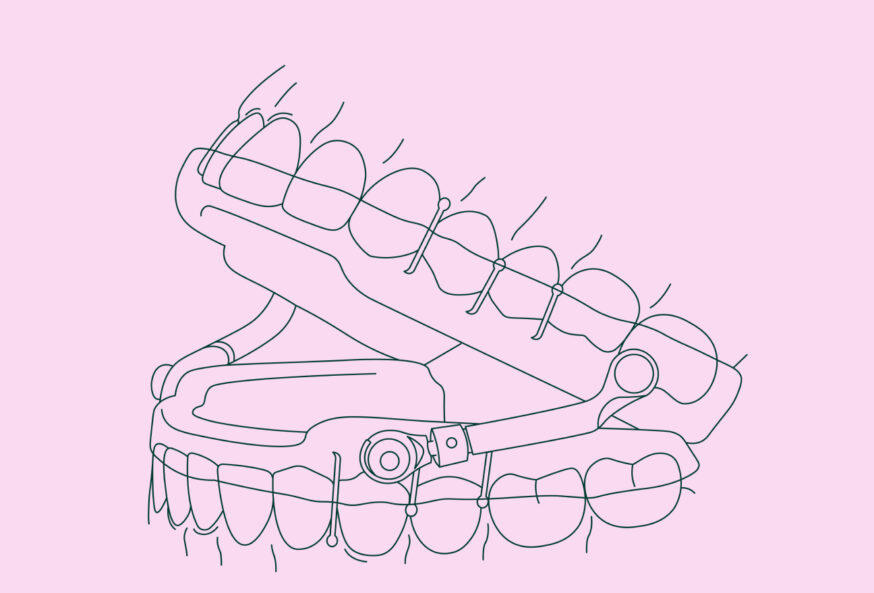
Dorsal appliances
A dorsal sleep apnea appliance is a two-piece appliance. The lower jaw is held in the correct position while allowing considerable jaw movement for the patient. The upper section has adjustable segments to control how much the lower jaw is advanced. The device has a dorsal fin that engages the maxillary and mandibular components and ensures the lower jaw stays in place during sleep.
Herbst appliances
A Herbst sleep apnea appliance is another type of oral appliance used to treat sleep apnea. The Herbst appliance was invented in 1909 by Dr. Emil Herbst (1872–1940). It’s a mandibular repositioning device originally designed to correct Class II malocclusion. The device has been improved in recent years and is a popular choice for treating sleep apnea, bruxism, TMJ, and chronic snoring. Known for its flexibility, the Herbst appliance allows the patient to maintain their full range of motion, including movement from side to side.
Setting the patient up for success with an oral sleep apnea appliance
The oral appliance will only work for sleep apnea if the patient uses it, an obvious thought but one to always consider. While a patient won’t spit out a crown, it is important to make sure they adhere to the plan. A partnership between physicians and qualified dentists in sleep apnea treatment is essential. The physician will confirm the diagnosis and may recommend oral appliance therapy (OAT). The dentist will confirm that treatment is appropriate and begin patient therapy. Both the dentist and the physician perform follow-ups with each medical professional providing their unique expertise, ensuring thorough patient communication throughout enabling that they stick to the treatment.
Explore Dandy’s custom 3D-printed oral sleep apnea appliances to treat your patients.
Join 15,000 dental professionals who get our emails every week
We send emails on Tuesdays. Keep an eye out for the next one!