A dentist’s journey adding sleep apnea treatment
Can dentists play a role in diagnosing sleep apnea?
The answer is a resounding “Yes,” dental can play a significant part in helping a patient get diagnosed with sleep apnea. Dentists, however, can’t technically diagnose patients for sleep apnea but they can facilitate the sleep study and referral to a sleep-focused physician. This is a collaborative effort as the sleep physician reads the sleep study and will prescribe a sleep apnea oral service based on the results.
Dentists can play an important role and help get all of this to transpire. It’s a collaboration to get patients to move forward and treat their sleep apnea properly.
Depending on various factors, this treatment of choice can be a mandibular advancement oral sleep appliance or another oral device. These appliances are fitted by the dentist. Not the physician.
Dentistry’s involvement in alleviating sleep apnea has become increasingly prominent. As a result, the awareness of these sleep apnea dental devices to unobstruct the airway has grown, and many digital dental labs can manufacture these appliances for dentists to help their patients and partners rest soundly and ultimately be healthier.
Dentists must examine the patient intra-orally, extra-orally, and with a comprehensive medical history. For example, when a patient reports snoring, not feeling alert, refreshed, and not dreaming, these can all be symptoms of obstructive sleep apnea.
Bruxism and sleep apnea can also be very tied together. Patients will often grind their teeth and move their jaw and tongue forward in an attempt to unobstruct their airway. They are trying to provide enough air space to breathe during sleep. This can be a fight-or-flight response as the patient fights for air. They may even be gasping for breath.
This nighttime bruxism can create attrition, loss of vertical dimension, headaches, sore muscles, TMD, etc.
Other signs include a high vaulted palatal arch, mouth breathing, a sizeable scalloped tongue, or retruded mandible. When these signs are presented, referring the patient for a sleep study and being adequately diagnosed for potential sleep apnea is recommended.
Simplistically, as “doctors of the mouth,” we dentists have a major role in helping with a patient’s sleep apnea diagnosis, and with oral appliances, we can treat the issue.
What is sleep apnea?
A patient may have sleep apnea when they pause or stop and start breathing for 10 seconds or more while asleep. This can be a very serious condition if gone untreated.
These abnormal events can be partial or shallow loss of breath or hypopnea, or total loss of breath, apnea. If a patient has five to 14 events per hour it is considered mild sleep apnea; moderate is 15-29 events per hour, and severe sleep apnea is an Apnea Hypopnea Index of 30 or more events per hour.
It is typically appropriate for dentists to get involved in treating mild-to-moderate obstructive sleep apnea. In these obstructive cases, the airway is narrowed or closed off during sleep by the tongue and soft tissue of the throat. It can be treated with a CPAP, surgery, or a dental device for sleep apnea.
When you are awake, the muscles are tight, and the airway is open, but when you are asleep, your body should be fully relaxed except for the diaphragm; the tongue can fall back due to the muscles being fully relaxed. This can cause the air passageway to narrow or be completely closed off. The uvula and surrounding tissues can also vibrate, causing snoring.
A home sleep study is a quick and convenient way for a patient to get tested for sleep apnea in their home. First, a sleep specialist will read the report. Then, with a letter of medical necessity and prescription from the physician, Dentists can often treat their patients with a dental device if the report shows mild-to-moderate sleep apnea.
However, suppose the report depicts the patient to be in a severe category. In that case, they may need another sleep study done in a sleep lab situation and ultimately treated with CPAP or combination therapy with a dental device.
The role of dentists in sleep apnea diagnosis
Dentists can play a major role in helping a patient pursue getting a diagnosis of sleep apnea. Dentists look into their patient’s mouths and can examine the teeth, jaw anatomy, tongue, and throat every visit (at least twice a year). Some patients come in even more often when involved in restorative or periodontal treatment that can take several phases and weeks of care. There is good face-to-face time to discuss or see any signs or symptoms of sleep apnea. Compare this to primary care physicians that typically see their patients once a year and may only do a very quick intra-oral exam.
Dentists should also add specific sleep and airway questions to the patient’s medical history intake form. And if you are doing intraoral wellness scans with digital dentistry, sleep apnea should be part of the check-in. We can specifically collect information showing signs or symptoms of potentially needing a home sleep test and refer to a sleep specialist for the diagnosis of sleep apnea. The dentist plays a significant role in helping the patient be referred to a sleep specialist and diagnosed.
The importance of screening for sleep apnea
Most patients do not visit their dentist’s office to ask about sleep apnea. They may be surprised that a dentist is even asking them questions about their sleep quality. That is where our dental screenings and wellness scans come into play. They are designed to extract enough information and create a conversation about the potential need for the patient to get a sleep study and get diagnosed with sleep apnea.
These screenings are so important. Ultimately we want to help our patients live longer and feel better because a person suffering from undiagnosed sleep apnea has higher risks of cardiovascular disease, high blood pressure, stroke, diabetes, daytime sleepiness, obesity, impaired cognition, irritability, mood disorders, and more. In addition, if dentists don’t screen for sleep apnea, it may go undiagnosed for an extended period, which is unsuitable for the patient’s overall health.
Symptoms of sleep apnea
Symptoms can range from nighttime sweating, excessive daytime sleepiness, not feeling refreshed in the morning, headaches, gastric reflux, lack of dreaming, frequent urination, and snoring. Some patients may report they have to have that extra few cups of coffee to get through the day, take frequent naps, or worse, fall asleep at the wheel while driving.
Explanation of common sleep apnea symptoms
When the tongue and soft tissue in the throat get obstructed, there can be episodes when the patient is not getting oxygen to the heart, brain, and organs.
- Headaches, from not being refreshed or getting enough blood to their brain or from bruxing
- Gastric reflux can be caused by stomach acid being pushed up into the esophagus.
- Daytime sleepiness due to not getting through all the stages of reparative sleep throughout the night. You also can’t go through all of the vital phases of sleep cycles to get the most and not get fully restful regenerative sleep which can cause daytime sleepiness, mood irritability, or anxiety.
- Snoring is the sound that a partially collapsed airway makes. The air vibrates the soft tissue of the airway.
- Mouth breathers may have red, inflamed gums due to dry mouth.
Discussion of how symptoms can be discovered by dentists
Dentists can start the evaluation of symptoms as soon as the patient walks in the door and into the waiting room. For example, do they have a narrow jaw or retruded mandible, or when they start talking, see if they appear skeletally Class 2? Do they sound winded, have bags under their eyes, or appear overweight and have a large neck circumference? These discoveries can be made even before the patients sit in the dental chair and open their mouths.
Dental factors in sleep apnea diagnosis
Dental factors that can contribute to sleep apnea
The size and position of the tongue can be significant contributors to sleep apnea.
Large scalloped tongue or tongue thrusting are signs of the patient trying to adjust their jaw by grinding to help them protrude their jaw and open throat space so they can move their tongue out of the way and breathe. The tongue gets indentations of the lingual embrasures as it continuously gets pressed against the teeth during this process.
The size of the arch is also crucial. A nicely arched wide dentition will allow the tongue to rest up and forward on the palate. However, if the jaw and palate are too narrow or retruded, there is no room to house the tongue, and it can fall back during sleep and obstruct the airway.
Bruxism and sleep apnea
Bruxism, muscle tension, and attrition are common signs of patients suffering from undiagnosed sleep apnea. The body is not getting enough air during apneic or hypopnea events. We respond by activating into fight or flight mode, and the body fights for air to survive. We are trying to open our airways by grinding our teeth forward to push the jaw and tongue forward. This can result in attritional pits on molars or incisor wear, or the loss of vertical dimension.
Many patients may blame this clenching and grinding just due to stress, but if you are sleeping and the body is relaxed, why would someone be grinding and a child be doing this? Some children don’t yet have the mental stress that adults do; they are also bruxing and fighting for air. The teeth may be sliding and grinding forward to open up the airway.
Referring patients to sleep studies
Based on the patient’s medical history, and intra-oral and extra-oral exams, I will ask if they have had a recent sleep study done. If not, I will link them to an online sleep company with a nationwide network of sleep physicians that provides cost-effective consultation, testing, diagnosis, and recommended treatment for sleep disorders. Many groups like this will dispense the home sleep study right to the patient’s home for use that night. The sleep data will be uploaded to a board-certified sleep specialist that will be ready to diagnose based on the sleep report. The specialist will typically recommend a CPAP and/or sleep device depending on the severity of the sleep apnea. If it is a mild or moderate case, they may send the dentist a letter of medical necessity for a dental appliance.
Types of dental sleep apnea treatments
The most common treatment is CPAP or a continuous positive airway pressure device. These machines blow consistent air into the patient’s airway through the nose or mouth.
There are also forms of surgery that can remove the tonsils, adenoids, uvula, and other soft tissue in the back of the throat to minimize airway obstruction. Implantable devices can also be surgically placed to send signals to the jaw muscles and tongue to prevent obstruction.
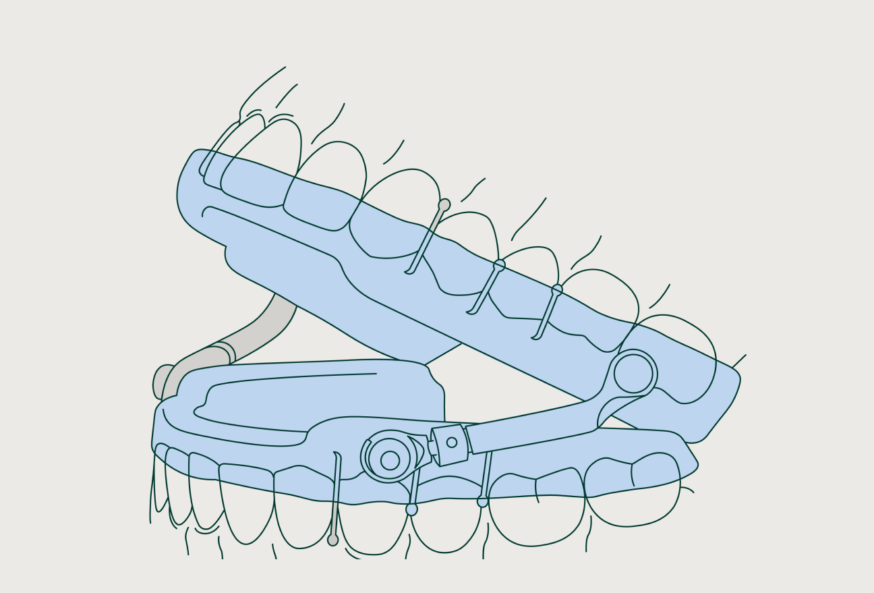
Dentists are involved with oral appliance therapy or mandibular advancement devices that shift the mandible and tongue forward and away from obstructing the throat.
Sleep apnea oral appliances
There are many different types of custom-fitted sleep apnea oral appliances. Some are all-acrylic with nylon or thicker rubber straps, but the most popular contain an upper tray, a lower tray, and a connector that hinges the mandible forward. In addition, most are adjustable to allow for titration regarding the amount of mandible protrusion.
The collaborative approach to sleep apnea treatment
Only a physician can diagnose OSA, but they may not look into the patient’s mouth or recognize the common oral facial signs and symptoms as much as dentists do. Therefore, a collaborative approach is in the best interest of the most critical person regarding sleep apnea, the patient. Especially with children, when sleep apnea is suspected, there needs to be a collaborative effort with the primary care physician, pediatric ENT, orthodontist, etc.
How dentists work alongside other healthcare providers to provide sleep apnea services
When it comes to treating patients for sleep and airway, it is not just about helping them with their teeth. It is helping them with their overall health and across several specialties of medicine, such as the dentist helping the patient by treating alongside primary care physicians, cardiologists, pulmonologists, sleep physicians, ENTs, pediatricians, Orthodontists, myofunctional therapists, etc. When patients lack proper oxygen or blood flow to their organs, the entire body is affected, not just the mouth.
Overview of benefits of a collaborative approach to treatment
Sleep apnea treatment is multifactorial. It is not just one form of medicine or dentistry. It is many. We have to be like a detective reviewing a crime scene. Doctors must come together to determine the best treatment for the patient. Snoring and sleep apnea will be among the most rewarding treatments you can offer your patients and community. While it does take partnering with physicians, the rewards of care are crucial to your patients, not to mention your practice’s bottom line.
With digital dentistry, dentists can scan, order, and fit 3D oral appliances to alleviate sleep apnea. Once you add to your practice, talk to your staff about incorporating sleep apnea questions into your workflow, be it part of the check-in, cleanings, or wellness scans.
Sleep apnea appliances with Dandy
Adding sleep apnea treatment to your dental practice is simple with Dandy and allows you to grow your practice’s value-per-patient exponentially. Dandy offers both Herbst and Dorsal appliances as well as education on medical billing. Explore Dandy’s custom 3D-printed sleep apnea appliances to treat your patients.