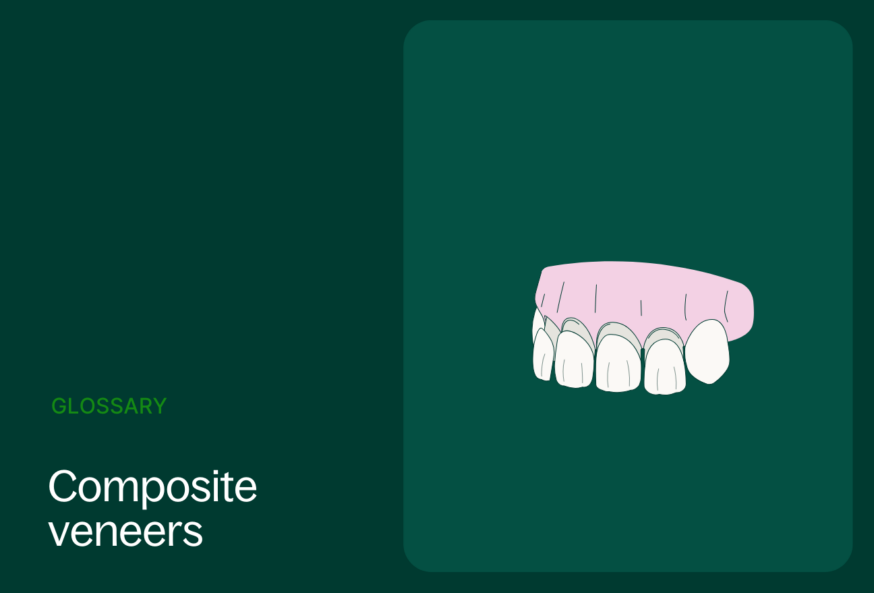
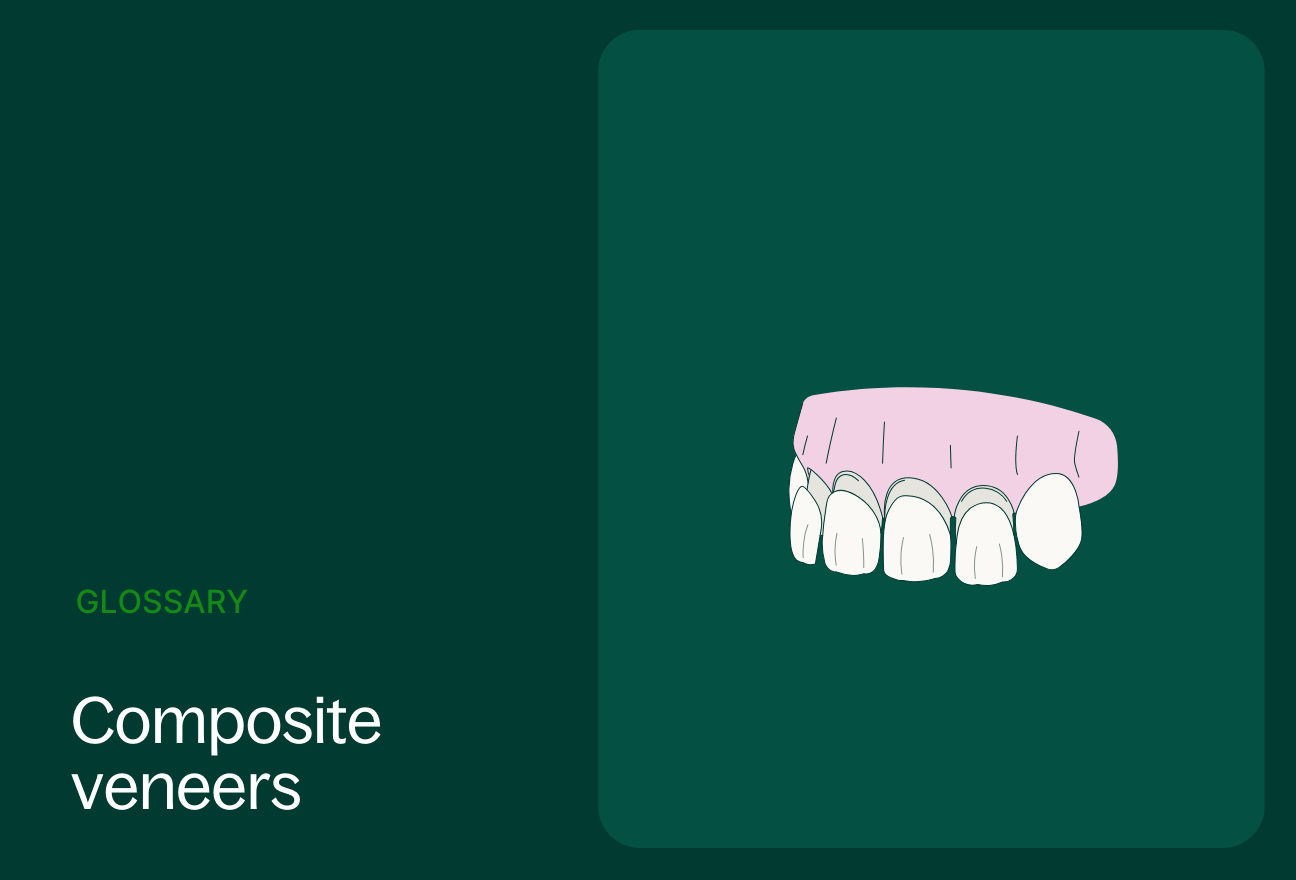
Composite veneers are thin shells made of tooth-colored resin that are bonded to the front surface of a patient’s teeth to improve their appearance. They are a more affordable and less invasive alternative to porcelain veneers, and they can be used to correct a variety of cosmetic problems including staining, chips or cracks, and misaligned teeth.
Composite veneers materials
There are two main materials of composite veneers, each using a different type of resin.
- Bisphenol A-glycidyl methacrylate (Bis-GMA): This is the most common type of resin used for composite veneers. It is a strong and durable material that can be bonded well to teeth. However, Bis-GMA can release small amounts of BPA, a chemical that has been linked to some health concerns.
- Urethane dimethacrylate (UDMA): This is a newer type of resin that is less likely to release BPA (Bisphenol A) than Bis-GMA. It is also a strong and durable material, and it can be bonded well to teeth.
Other materials that may be used in composite veneers include:
- Silica is a filler that helps to strengthen the composite resin and make it more resistant to wear.
- Zirconium is another filler that is sometimes used in composite veneers. It is similar to silica, but it is stronger and more resistant to chipping.
- Glass is sometimes used as a filler in composite veneers. It can help to make the veneers more translucent and give them a more natural appearance.
The specific materials used in composite veneers will vary depending on the manufacturer and the dentist’s preferences. However, all of the materials used in composite veneers are safe and effective.
Workflow for composite veneers
Applying composite veneers is a relatively simple, four-step process.
- Consultation: During the consultation, the patient will discuss their goals for their smile with you. After an examination of the patient’s teeth and gums, it can be determined if they are a good candidate for composite veneers. You, the dentist will also determine which type of composite veneer is the most apt for the patient during the consultation.
- Veneer Preparation: On the day of the procedure, you will begin by preparing the patient’s teeth for the veneers by removing a thin layer of enamel to create space for the veneers and to ensure a good bond between the veneers and the teeth.
- Application: Once the teeth are prepared, apply the composite resin to the front surface of the teeth. The resin will be sculpted to the desired shape and size, and it will be cured with a special light.
- Polishing: Once the resin is cured, polish the veneers to give them a natural shine.
Direct composite veneers
Once known as “day savior fillings,” as they can be done in one patient visit, direct composite veneers have evolved into becoming reliable, durable and minimally invasive solutions for smile makeovers for the right patient. A study published by the National Library of Medicine showed that after two years direct composite ventures proved themselves to be one of the most promising treatment options for patients.
Direct composite veneers workflow
The workflow for direct composite veneers can be summarized in the following steps:
Preoperative evaluation and diagnosis
- Initial consultation: Gather patient’s history, expectations, and aesthetic concerns. Perform a thorough clinical examination to assess oral health, tooth alignment, and bite function.
- Diagnostic records: Take dental impressions (digital preferred), photographs, and radiographs to evaluate tooth structure, occlusion, and underlying bone support.
- Treatment planning: Discuss treatment options with the patient, considering factors such as patient preference, budget, and severity of aesthetic defects.
Tooth preparation and etching
- Anesthesia: Apply local anesthesia to the treatment area to numb the teeth and surrounding tissues.
- Rubber dam isolation: Place a rubber dam to isolate the treatment area, preventing saliva contamination and ensuring a dry field.
- Tooth preparation: Minimal enamel preparation is required to create a bonding surface for the composite resin. This involves using fine burs to remove a thin layer of enamel, typically 0.5-1.0 millimeter.
- Acid etching: Etch the enamel surface with phosphoric acid for 30 seconds to create microscopic pores, enhancing the adhesion of the composite resin to the tooth structure.
Bonding and layering composite resin
- Primer application: Apply a primer to the etched enamel surface to increase bonding strength.
- Adhesive application: Apply a thin layer of adhesive resin to both the tooth surface and the composite resin.
- Light curing: Polymerize the adhesive resin using a curing light to create a strong bond between the tooth and the composite resin.
- Composite resin layering: Build up the composite resin in incremental layers, starting with an opaque dentin shade to mask the underlying tooth color.
- Coloration and characterization: Use different shades and translucency levels of composite resin to create natural-looking tooth contours, mamelons, and incisal edges.
- Additional light curing: After each layer of composite resin is placed, it is carefully cured with a curing light to ensure proper polymerization and prevent premature bonding failure.
Finishing and polishing
- Initial shaping: Use fine diamond burs or carbide burs to shape the composite resin into the desired tooth anatomy.
- Finishing: Refine the surface texture of the composite resin using polishing discs and polishing strips to achieve a smooth and natural-looking finish.
- Occlusal adjustment: Evaluate and adjust the occlusion to ensure proper bite function and prevent premature tooth wear.
- Final polishing: Apply polishing paste with a polishing wheel to achieve a high-gloss finish that mimics the natural shine of enamel.
Postoperative care and follow-up
- Postoperative instructions: Provide the patient with postoperative care instructions, including dietary recommendations and oral hygiene guidelines.
- Follow-up appointments: Schedule follow-up appointments to monitor the healing process, evaluate the aesthetics and function of the veneers, and provide any necessary adjustments or maintenance.
Direct composite veneers indications
- Mild to moderate tooth discoloration: Composite veneers can effectively mask tooth discoloration caused by tetracycline staining, fluorosis, or mild general staining.
- Minor tooth misalignment: Direct composite veneers can be used to correct minor tooth misalignment, such as crowding, spacing, or mild rotations.
- Chipped or fractured teeth: Composite veneers can restore the aesthetics and function of chipped or fractured teeth, especially in the anterior region.
- Abraded or eroded teeth: Direct composite veneers can protect abraded or eroded teeth from further wear and enhance their appearance.
- Diastemas: Composite veneers can effectively close diastemas, which are gaps between teeth.
- Aesthetic contouring: Direct composite veneers can be used to improve the overall appearance of teeth by modifying their shape, size, and contour.
Direct composite veneers contraindications
- Severe tooth discoloration: Direct composite veneers may not be able to adequately mask severe tooth discoloration caused by factors such as endodontic treatment or extensive metallic restorations.
- Significant tooth misalignment: For moderate to severe tooth misalignment, orthodontic treatment is often a more appropriate option.
- Major tooth wear or loss of tooth structure: Direct composite veneers may not be strong enough to restore teeth with significant wear or loss of tooth structure.
- Poor oral hygiene: Patients with poor oral hygiene are at increased risk of composite veneer fracture or failure.
- Bruxism: Patients with bruxism, or excessive grinding of teeth, may require protective nightguards to prevent damage to the composite veneers.
- High bite forces: Direct composite veneers may not be suitable for patients with high bite forces, especially in the posterior region.
- Unrealistic expectations: Patients should have realistic expectations about the aesthetic outcome of direct composite veneers.
- Allergy to composite resin materials: Patients with a known allergy to composite resin materials should not undergo this procedure.
Indirect composite veneers
Indirect composite veneers are a type of cosmetic dental restoration that is used to improve the appearance of teeth. They are made from a composite resin material that is layered onto a model of the patient’s teeth. The veneers are then bonded to the teeth, providing a durable and natural-looking restoration.
Indirect composite veneers workflow
The workflow for indirect composite veneers typically involves the following steps:
Preoperative evaluation and diagnosis
- Initial consultation: Gather the patient’s history, expectations, and aesthetic concerns. Then perform a thorough clinical examination to assess oral health, tooth alignment, and bite function.
- Diagnostic records: Take dental impressions (digital preferred), photographs, and radiographs to evaluate tooth structure, occlusion, and underlying bone support.
- Treatment planning: Discuss treatment options with the patient, considering factors such as patient preference, budget, and severity of aesthetic defects.
Tooth preparation and impression
- Anesthesia: Apply local anesthesia to the treatment area to numb the teeth and surrounding tissues.
- Rubber dam isolation: Place a rubber dam to isolate the treatment area, preventing saliva contamination and ensuring a dry field.
- Tooth preparation: Minimal enamel preparation is required to create a bonding surface for the composite resin. This involves using fine burs to remove a thin layer of enamel, typically 0.5-1.0 millimeter.
- Impression: Take a high-quality impression of the prepared teeth.
Laboratory fabrication of the veneer
- Model creation: Pour the impression material into a stone cast to create a working model of the patient’s teeth.
- Wax-up: Wax is sculpted onto the model to create the desired shape and anatomy of the veneer.
- Investing: The wax-up is covered in an investment material and placed in a furnace to create a mold.
- Composite resin application: Composite resin is carefully layered into the mold, following the contours of the wax-up.
- Pressurization: The mold is pressurized to ensure proper compaction of the composite resin.
- Curing: The composite resin is cured under ultraviolet light to harden the material.
- Finishing and polishing: The veneer is finished and polished to achieve a natural-looking surface.
Veneer placement
- Try-in: The veneer is placed on the tooth to check for fit and aesthetics.
- Bonding: The tooth surface is etched with acid to create a micromechanical bond.
- Adhesive application: A bonding agent is applied to both the tooth and the veneer.
- Luting: The veneer is bonded to the tooth using a light-cured composite resin.
- Marginal adaption: Excess composite resin is removed, and the margins are polished to create a smooth transition between the veneer and the natural tooth.
- Occlusal adjustment: Evaluate and adjust the occlusion to ensure proper bite function and prevent premature tooth wear.
- Final polishing: Apply polishing paste with a polishing wheel to achieve a high-gloss finish that mimics the natural shine of enamel.
Postoperative care and follow-up
- Postoperative instructions: Provide the patient with postoperative care instructions, including dietary recommendations and oral hygiene guidelines.
- Follow-up appointments: Schedule follow-up appointments to monitor the healing process, evaluate the aesthetics and function of the veneers, and provide any necessary adjustments or maintenance.
Indirect composite veneers indications
- Moderate to severe tooth discoloration: Indirect composite veneers can effectively mask moderate to severe tooth discoloration.
- Significant tooth misalignment: Indirect composite veneers can be used to correct significant tooth misalignment, such as moderate to severe crowding, spacing, or rotations.
- Major tooth wear or loss of tooth structure: Indirect composite veneers can restore teeth with significant wear or loss of tooth structure.
- High bite forces: Indirect composite veneers are stronger than direct composite veneers and may be a better option for patients with high bite forces.
Indirect composite veneers contraindications
- Poor oral hygiene: Patients with poor oral hygiene are at increased risk of composite veneer fracture or failure.
- Bruxism: Patients with bruxism may require protective nightguards to prevent damage to the composite veneers.
- Unrealistic expectations: Patients should have realistic expectations about the aesthetic outcome of indirect composite veneers.
- Allergy to composite resin materials: Patients with a known allergy to composite resin materials should not undergo this procedure.
How long do composite veneers last?
Composite veneers can typically last for five-to-seven years. However, several factors can affect their longevity, including:
- Oral hygiene: Good oral hygiene is essential for prolonging the life of composite veneers. This includes brushing your teeth twice a day, flossing daily, and using a mouthwash.
- Diet: A diet that is high in sugar and acid can damage composite veneers. Limit your intake of sugary drinks, candy, and acidic foods.
- Grinding your teeth: If you grind your teeth, you may need to wear a nightguard to protect your veneers from damage.
- Smoking: Smoking can stain and damage composite veneers. If you smoke, quitting is the best way to protect your veneers.
The material used in composite veneers can significantly impact their longevity. Composite veneers are made from a resin-based material that is bonded to the tooth surface. The type of resin used, as well as the quality of the bonding process, can affect how long the veneers last.
- Microfill: Microfill composite resins have very fine particles, which makes them more durable and less likely to chip or crack. However, they are also more difficult to polish to a high shine.
- Macrofill: Macrofill composite resins have large particles, which makes them less durable and more likely to chip or crack. However, they are also the easiest to polish to a high shine.
- Hybrid: Hybrid composite resins are a mixture of microfill and macrofill particles. They are more durable than macrofill resins, but they are less durable than microfill resins. They are also easier to polish than microfill resins.
Composite veneers vs. porcelain veneers longevity
Composite veneers have an average lifespan between five and seven years, whereas porcelain veneers have a lifespan between 10 and 15 years. If longevity is the main factor in consideration, porcelain veneers are generally a better choice for patients who want the most natural-looking, durable, and long-lasting veneers. However, composite veneers are a good option for patients who are on a budget or who want a less invasive procedure.
Comparison between direct composite and indirect composite workflows
There are many factors to be considered when choosing which type of composite veneers are right for a patient. Among them are price, aesthetics, and complexity of the procedure. The best workflow for you will depend on your individual needs and preferences. Indirect composite veneers require multiple steps more than the direct composite option, including the lab fabrication from an intraoral scan dental impression. The application of indirect composite veneers will often take at least two-to-three visits while direct composite veneers can be installed within a matter of a couple of hours during a single visit. The extended process is often worth it as indirect composite veneers are more aesthetically pleasing and more durable than direct composite veneers.
What are composite veneers made out of?
Composite veneers are made out of a tooth-colored resin material. This resin is composed of several different components, including:
- Fillers: Fillers are the main component of composite resin. They are typically made of glass or ceramic particles and give the resin its strength and durability.
- Monomer: Monomer is the liquid component of composite resin. It is responsible for bonding the fillers together and creating a hard, durable surface.
- Initiator: Initiator is a chemical that is used to start the polymerization reaction. This reaction hardens the resin and makes it more durable.
- Inhibitor: Inhibitor is a chemical that is used to slow down the polymerization reaction. This is important because it allows the dentist to sculpt the resin before it hardens.
- Pigments: Pigments are added to the resin to give it a natural tooth-like color.
The specific composition of composite resin varies depending on the manufacturer. However, all composite resins contain these basic components.
What are porcelain veneers?
Porcelain veneers are thin, custom-made shells of tooth-colored material designed to cover the front surface of teeth to change their appearance. They are made of a high-grade ceramic material that is strong, durable, and resistant to staining. Porcelain veneers are often considered to be the best option for cosmetic dental restorations because they can provide a natural-looking and long-lasting solution for a variety of dental problems.
Benefits of porcelain veneers
- Natural-looking appearance: Porcelain veneers are very closely matched to the natural color and translucency of teeth, so they can give teeth a very natural-looking appearance.
- Durability: Porcelain veneers are very strong and durable, and they can resist chipping and cracking.
- Stain resistance: Porcelain veneers are resistant to staining, so they can help to keep teeth looking white and bright.
- Versatility: Porcelain veneers can be used to correct a variety of dental problems, including:
- Chipped or cracked teeth
- Discolored teeth
- Gaps between teeth
- Crooked or misaligned teeth
- Shortened teeth
Workflow for porcelain veneers
The procedure for installing porcelain veneers involves the following steps:
- Consultation: The first step is to have a consultation with the patient to discuss their goals for treatment and determine if porcelain veneers are the right option.
- Tooth preparation: The dentist will remove a small amount of enamel from the front of the teeth to make room for the veneers.
- Impressions: Impressions will be taken of the teeth to create custom-made veneers.
- Temporary veneers: While the permanent veneers are being made, the patient may be given temporary veneers to wear.
- Veneer placement: The permanent veneers will be bonded to the teeth using a special adhesive.
- Final touches: The dentist will trim and polish the veneers to ensure they look natural and fit perfectly.
Porcelain veneers vs. composite veneers
The best type of veneer for you will depend on the individual needs and goals of the patient. Porcelain veneers are the best choice if the patient prioritizes durability and the most natural look. However, if they are on a budget or want a less time-consuming procedure, then composite veneers may be the better option.
Here is a summary of the key differences between porcelain veneers and composite veneers:
- Material: Porcelain veneers are made of a ceramic material, while composite veneers are made of a tooth-colored resin.
- Appearance: Porcelain veneers are generally considered to be more natural-looking than composite veneers.
- Durability: Porcelain veneers are more durable than composite veneers.
- Stain resistance: Porcelain veneers are more stain resistant than composite veneers.
- Cost: Porcelain veneers are more expensive than composite veneers.
- Procedure: The procedure for getting porcelain veneers is more time-consuming than the procedure for getting composite veneers.
- Reversibility: Porcelain veneers are less reversible than composite veneers as the latter bonds to the teeth but does not remove enamel.
Are composite veneers right for your practice?
Composite veneers offer a couple of benefits over porcelain veneers. Porcelain veneers are more durable and natural-looking than composite veneers, but those benefits come with a cost—the process is far more time-consuming and expensive. You will most likely want to nudge patients who are looking to have a less invasive, more reversible, and less expensive procedure toward composite veneers.